|
|
|
|
|
|
Provider Services 1-833-644-6001 |
|
|---|
|
|
Remittance advice payment recovery details available
Due to the Change Healthcare/Optum security incident, remittance advices generated after February 21, 2024, have not included certain claim recovery information.
AmeriHealth Caritas Ohio is pleased to inform you that a solution has been developed in collaboration with Change Healthcare/Optum to provide the detailed payment recovery information missing from the provider remittance advice. This solution will provide payment recovery details on the remittance advice or 835 you receive with your payments for claims processed on and after May 6, 2024.
For claims processed February 21, 2024, through May 5, 2024, AmeriHealth Caritas Ohio has generated a comprehensive claims recovery report available in the NaviNet provider portal. The claims recovery report provides payment recovery details by your member account number, claim number, provider tax ID, payee/group ID, and NPI.
To access the claims recovery report:
- Log in to the NaviNet provider portal
- Select applicable health plan.
- Go to
Report Inquiry, under
Workflows for this Plan.
- Click on
Administrative Reports>Claim Recovery Report.
If you do not have access to the NaviNet provider portal, please visit: https://register.navinet.net/ to sign up.
Questions: Please contact your Provider Network Management Account Executive or Provider Services at 1-833-644-6001. We appreciate your partnership and patience as we work to re-establish services and will continue to share additional information as it becomes available. |
|
|---|
|
 Ohio Department of Medicaid updates Ohio Department of Medicaid updates |
|
|---|
|
New features implemented in the Ohio Medicaid Enterprise System
The New Features Implementation Overview outlines key changes for providers.
Medicaid’s Office of Behavioral Health Policy 2024 rate increases
July 1 Electronic Visit Verification program changes
Ohio Administrative Code (OAC) rule 5160-1-40
Sandata Mobile Connect application updated
The Sandata mobile application has been replaced with a new and improved version.
Sandata Mobile Connect - Google Play Store
Sandata Mobile Connect - Apple Store
ODM authorizing $10 million to help at-risk youth across Ohio
Read the press release.
Reimbursement information
ODM released tools that explain the MCE claims and PA denials processes.
Medicaid agreement revalidations
To complete revalidation, visit PNM & Centralized Credentialing.
SL modifier not required for Vaccines for Children (VFC) Program
As of April 30, the VFC program no longer requires the use of the SL modifier for claims reimbursement.
Updated rates
The new rates are available on ODM's website.
Update your specialties page in Provider Network Management module
See the Specialty Quick Reference Guide for instructions.
Updated HEDIS guidelines for the Care Gap Closure program
View the HEDIS 2023 Documentation and Coding Guidelines for care delivered in 2024.
Ohio Department of Medicaid fraud warning
If your Medicaid patient is contacted for their personal information, advise them to not respond. Report it to the Ohio Attorney General at 1-800-282-0515 or via the online form.
Incomplete PNM affiliation steps may impact provider billing
An Affiliations Quick Reference Guide has been created with step-by-step instructions
New administrator change form
A new form must accompany requests to change PNM Administrators from one billing organization provider to another.
Updated claim submission and adjudication FAQ
Claims and Prior Authorization Submission Frequently Asked Questions (FAQ).
EPSDT- HEALTHCHEK annual education as required by ODM
The Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit provides comprehensive and preventative healthcare services for children under age 21 who are enrolled in Medicaid. EPSDT is key to ensuring that children and adolescents receive appropriate preventative, dental, mental health, developmental, AND specialty services.
Screenings Must Include:
- Comprehensive Health and Developmental History
- Comprehensive Unclothed Physical Exam
- Laboratory Tests – Including Lead Toxicity Screening as guided by the child’s age
- Appropriate and needed immunizations
- Health Education – Anticipatory Guidance including Child Development, Healthy Lifestyles, and Accident and Disease Prevention
- Vision Services – at minimum, diagnosis and treatment for defects in vision, including eyeglasses
- Dental Services – at minimum, relief of pain and infections, restoration of teeth, and maintenance of dental health
- Hearing Services – at minimum, diagnosis and treatment for defects in hearing, including hearing aids
- Nutrition assessment and education
- Other Necessary Health Care Services – diagnostic and treatment services must be provided when a screening examination indicates the need for further evaluation
Email links
|
|
 Resources and reminders Resources and reminders |
|
|---|
|
Need help?
Reminder to providers regarding overpayments
AmeriHealth's Claims Cost Containment Unit is responsible for the manual review of overpaid claims submitted by the Program Integrity department for potential recovery. Claims submitted to the Claims Cost Containment Unit for review are outside of the Subrogation and Check Reconciliation areas. Some examples of identified waste include:
- Incorrect billing from providers causing overpayment
- Overpayment due to incorrect set-up or update of contract/fee schedules in the system
- Overpayments due to claims paid based upon conflicting authorizations or duplicate payments
- Overpayments resulting from incorrect revenue/ procedure codes, retro TPL/Eligibility
The Claims Cost Containment Unit is also responsible for the manual review of provider-initiated overpayments. Providers who self-identify claim overpayments may submit their inquiries for review to:
AmeriHealth Caritas Ohio
Attn: Claims Cost Containment
PO Box 7320
London, KY 40742
Further information can be found on pages 115 through 117 of the AmeriHealth Caritas Ohio Provider Manual.
Reminder to providers regarding urine drug screening
Drug screen testing detects the presence of drugs or drug classes in a patient’s system during an encounter. The results are reported as positive or negative for the presence of a drug or drugs but do not indicate specific levels. The tests provide information about recent drug use but do not distinguish between occasional users and those who are dependent on or otherwise impaired by drug use.
Drug screen testing includes:
- Presumptive drug class screening used to identify possible use or non-use of a drug or drug class. It is done on a random basis or for cause, the latter of which should be documented in the medical record. In substance use disorder treatment settings, presumptive testing should be a routine part of initial and ongoing patient assessment.
- Definitive drug class screening comprised of qualitative (drug is present or absent), semi-quantitative, or quantitative (measured) tests to identify possible use or non-use of a specific drug; typically, therapeutic drug assay procedures are quantitative tests. Definitive testing may be used to detect specific substances not identified by presumptive methods and to refine the accuracy of the test results when the results are needed to inform clinical decisions.
Drug testing should supplement information obtained by history and physical examination and should never be the sole basis for making a diagnosis of a substance use disorder (American Society of Addiction Medicine, 2019). Drug testing should be performed for individuals who would be helped most by such screens. Routine drug screening in the absence of clear clinical suspicion for illicit use should be avoided. Choice of test matrix, selection, and frequency should fit the needs of the tested population, with more intense and less predictable testing reserved for persons at highest risk of drug use (American Society of Addiction Medicine 2019, Manchikanti, 2012).
AmeriHealth follows OAC rules associated with presumptive and definitive drug screens.
- For presumptive screens, thirty dates of service per benefit year; and
- For definitive tests, twelve dates of service per benefit year.
PNM portal
Until it is fully active, please continue to send roster updates to both PNM and the MCO’s. Behavioral Health providers ARE able to only update through the PNM portal without submitting rosters to the MCO’s.
Medicaid annual eligibility redetermination reviews
Information for providers regarding Annual Eligibility Redetermination Reviews is on our website. This federally required process is in place to ensure those enrolled in Medicaid programs continue to meet established eligibility criteria. AmeriHealth Caritas Ohio will collaborate with Ohio Department of Medicaid and our provider network to minimize the burden on our members and promote continuity of health coverage.
Access and availability standards
As part of ongoing network management, periodic outreach to confirm maintenance of access and availability standards does occur. The specific access time frames are determined by the provider type of the service and is outlined starting on page 33 of the AmeriHealth Caritas Ohio Provider Manual.
Appointment availability
Thank you all for being such a valued part of our Provider Network! As we all know, the health and well-being of our Medicaid population is our focus and main reason for being. Having access to quality care is so important to our members, your patients. To ensure that this is a top priority, please review with your team the importance of availability of specialty care appointments. Federal guidelines require that providers support the following:
- Specialty Care Access Appointments - this is care provided for a non-emergent/non urgent illness or injury requiring consultation, diagnosis, and/or treatment from a specialist. These are to be made available within 6 weeks or less.
We appreciate all the time and effort you put in to ensure that your patients/our members receive the best possible care!
|
|
 Prior authorizations Prior authorizations |
|
|---|
|
Submit authorizations electronically through NaviNet
AmeriHealth Caritas Ohio offers our providers access to our Medical Authorizations portal for electronic authorization inquiries and submission. The portal is accessed through NaviNet and located on the Workflows menu.
In addition to submitting and inquiring on existing authorizations, you will also be able to:
- Verify if No Authorization is Required
- Receive Auto Approvals, in some circumstances
- Submit Amended Authorization
- Attach supplemental documentation
- Sign up for in-app status change notifications directly from the health plan
- Access a multi-payer Authorization log
- Submit inpatient concurrent reviews online if you have Health Information
- Exchange (HIE) capabilities (fax is no longer required)
- Review inpatient admission notifications and provide supporting clinical documentation
Prior authorization lookup tool
To find out if a service needs prior authorization, click here to get started.
Wait for the page to fully loadEnter a CPT or HCPCS code in the search box at the bottom of the pageClick SubmitThe tool will tell you if that service needs prior authorization
Removal of certain prior authorizations effective 6/22/24
Removal of prior authorization for certain services is part of our continued efforts to make the prior authorization process more efficient and transparent. Our goal is to enhance the provider experience by making it easier for providers to navigate the prior authorization process, helping ensure timely member access to necessary services.
Beginning 6/22/24, the procedure codes listed in Table 1 do not require prior authorization.
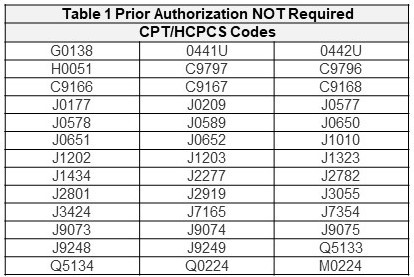
As a reminder, to verify whether a service requires prior authorization, use the Prior Authorization Lookup Tool on the provider website. Medications billed via the medical benefit (CMS 1500 or UB-04) are reviewed by our PBM, PerformRx. You can download a form here to submit via fax.
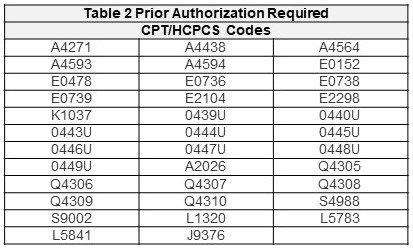
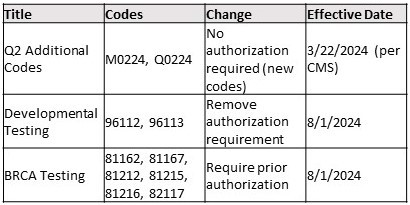
The following items were approved at the quarterly Prior Authorization Review Committee (PARC) meeting held on 6/26/2024.
Questions? Contact your Provider Network Management Account Executive or Provider Services at 1-833-644-6001.
|
|
 Claims and billing Claims and billing |
|
|---|
|
How to investigate a claim
- Log into NaviNet.
- On the Health Plans menu, under My Plans, click AmeriHealth Caritas Ohio.
- Under Workflows for This Plan, click Claim Status Inquiry, and then find your claim.
- On the Claim Details screen, above the status bar, click Claim Investigation. The Investigation Claim # pop-up window appears.
- Choose an investigation type, and then type your comments for the investigation reviewers. Claim investigations are per claim, not per line item. To reference a specific claim line, provide the line number in the Comments box.
- In the remaining boxes, type your contact information for this investigation so that customer service can contact you, if necessary.
- Click Submit.
A confirmation message appears. For example:
Your Investigation Request for Claim # 118833994 has been submitted to the plan.
Our goal is to respond to your inquiry within 7 days, however, at times due to volumes of complexity our response may take up to 30 days.
To check the status of your investigation after you submit it, click Claim Investigation Inquiry under Workflows for This Plan.
If you submit an investigation without required information, AmeriHealth Caritas Ohio cannot complete it. AmeriHealth Caritas Ohio responds to the investigation and notes the missing information. Click here for the NantHealth Help Center.
Consent forms
Providers must submit the appropriate required forms (ODM 03197, ODM 03199, HHS-687, and HHS687-1 [SPANISH VERSION]) with the claim’s submission for these services. Appropriate consent forms can be found on AmeriHealth Caritas Ohio's website or on the ODM website at Pregnancy Risk Assessment | Medicaid (ohio.gov). Providers can submit the consent form along with their claim through Change Healthcare:
- Submit a 275 claim attachment transaction. AmeriHealth Caritas Ohio is accepting ANSI 5010 ASC X12 275 unsolicited attachments via Change Healthcare. Please contact your Practice Management System Vendor or EDI clearinghouse to inform them that you wish to initiate electronic 275 attachment submissions via payer ID 35374.
There are three ways that 275 attachments can be submitted:
- Batch - you may either connect to Change Healthcare directly or submit via your EDI clearinghouse.
- API via JSON - you may submit an attachment for a single claim.
- Portal - individual providers can register at Change Healthcare to submit attachments.
The acceptable supported formats are pdf, tif, tiff, jpeg, jpg, png, docx, rtf, xml, doc, and txt. View the Change Healthcare 275 claims attachment transaction video for detailed instructions on this process. In addition, the following 275 claims attachment report codes have been added. When submitting an attachment, use the applicable code in field number 19 of the CMS 1500 or field number 80 of the UB04, as documented in the Claims Filing Instructions (PDF).
|
Attachment type
|
Claim assignment attachment report code
|
|
Itemized bill
|
03
|
|
Medical records for HAC review
|
M1
|
|
Single case agreement (SCA)/LOA
|
04
|
|
Advance beneficiary notice (ABN)
|
05
|
|
Consent form
|
CK
|
|
Manufacturer suggested retail price/invoice
|
06
|
|
Electric breast pump request form
|
07
|
|
CME checklist consent forms (child medical eval)
|
08
|
|
EOBs — for 275 attachments, should only be used for non-covered or exhausted benefit letter
|
EB
|
|
Certification of the Decision to Terminate Pregnancy
|
CT
|
|
Ambulance trip notes/run sheet
|
AM
|
No paper claims
The Next Generation of Ohio Medicaid program's guidelines require all claims to be submitted via the Electronic Data Exchange (EDI). Use AmeriHealth Caritas Ohio’s EDI Payer ID# 35374. You can get started on our website with claims how-tos, quick guides, links and contact info.
Correcting claims
Oops! What if I submitted claims with the wrong rate or CPT code? Please refer to our Provider Claims and Billing Manual on how to submit corrected claims on page 52.
Provider Claims and Billing Manual - Box 33, no PO Box allowed
Field: 33Field description: Billing provider Info and phone numberRequired - identifies the provider that is requesting to be paid for the services rendered and should always be completed. Enter the physical location; PO Boxes are not acceptable.
- Required fields must be completed on all claim
- Loop ID: 2010AA
- Segment: NM103, NM104, NM105, NM107, N301, N401, N402, N403, PER04.
See page 17 of the Provider Claims and Billing Manual.
Claims Payment Systemic Error (CPSE) report
The Claims Payment Systemic Errors (CPSE) report is updated and posted on the Alerts and Newsletter page monthly. AmeriHealth Caritas Ohio encourages you to review this log frequently and before contacting our Provider Services team. If you have additional questions, please feel free to reach out to Provider Services at 1-833-644-6001 and, as always, you can reach out to your local account executive.
Billing for hospital readmission
For prompt and accurate payment processing, please consult ODM's Hospital Guidance on Hospital Re-admissions found on page 31 of the Hospital Billing Guidelines.
Please note, that ODM instructs the following concerning re-admissions to a hospital: If a recipient is an inpatient in a hospital, is discharged, then subsequently re-admitted to the same hospital within a day, the hospital must collapse the two inpatient stays into one admit through discharge claim. The hospital must report one non-covered day at the header and use Revenue Code 180 to report a non-covered day at the detail. For example, if the recipient is hospitalized 1/1 and is discharged to a NF on 1/5, then re-admitted to the hospital on 1/6, the hospital must report one non-covered day for the first date of discharge (1/5) at the header, and one non-covered day at the detail level, RCC 180.Depending on which claim (hospital or NF) is paid first, the second claim will deny as a duplicate due to a systems configuration limitation that will not process two claims with overlapping dates of service (i.e., the day the patient is readmitted to the NF for 8 hours or more). As a workaround, if your claim is denied as a duplicate, please resubmit your claim via the 6653 process for manual review.
Diabetes self-management education enhanced reimbursement rates
AmeriHealth Caritas Ohio and the Ohio Managed Care Organizations (MCOs) are working collaboratively to make diabetes management easier for providers and their patients. Diabetes education and support for the use of continuous glucose monitors (CGMs) have proven to be effective in diabetes care management.
To facilitate increased utilization of these enhanced tools, AmeriHealth Caritas Ohio and the other MCOs will pay an enhanced rate to providers rendering Diabetes Self-Management Education (DSME) and billing the appropriate codes: G0108 and G0109. In addition, PA is not required for members who receive a covered CGM device through durable medical equipment (DME) providers or through their pharmacy. Providers must use HCPCS codes A4239 and E2103 for CGMs provided through DME.
Services rendered in 2023 should be submitted without delay to prevent denials.
For additional information regarding these updates, including who to contact at each MCO for questions, see the quick reference guide on our provider website.
NIA is becoming Evolent
Evolent (formerly National Imaging Associates, Inc.) has consolidated its various companies (Evolent Care Partner; NIA Magellan; Vital Decisions; Evolent Health Services, IPG; and New Century Health) under a single brand: Evolent. This branding change will have negligible impact on providers, but you will start to see logo switch outs from NIA to Evolent on materials. Providers should continue to use RadMD.com to obtain prior authorizations and for future updates. Phone numbers to reach Evolent will also remain the same as they were for NIA.
|
|
When should the provider submit an Appeal vs. Dispute? |
|
|---|
|
|
Item and Definitions
|
Timeframe
|
Contact Information
|
|
Appeal
Filed by the member or provider on behalf of the member (with a waiver), related to a denied Service/IP service (Prior Auth denials, Limit to service/Auth) when there is no claim on file.
|
60 days from the date of denial letter sent by UM.
|
Medical appeals may be submitted via:
Mail: AmeriHealth Caritas Ohio
Attn: Member Appeals Coordinator
PO Box 7346
London, KY 40742
Phone: AmeriHealth Caritas Ohio Member Services
1-833-764-7700
(TTY: 1-833-889-6446)
Secure contact form: https://apps.amerihealthcaritasoh.com/securecontact/index.aspx
|
|
Inquiry
Provider asking for more information on a claim and how it was processed.
|
None
If determined the claim can be adjusted, then the inquiry is a dispute and should follow that timeframe.
|
NaviNet portal (www.navinet.net)
|
|
Dispute (or Provider Claim Appeal)
Provider disagreeing with the way a claim was processed, paid, or denied.
ODM outlines the following categories of items that are considered a dispute:
- Claim Status
- Eligibility
- Other insurance
- Improper claim submission
- Overpaid/underpaid
- Provider not eligible to provide service
- Payment amount clarification
- Provider not credentialed
- Duplicate claim
- Timely filing
- Documentation issues
- Recoupments
- Prior Authorization
- Medical Necessity
- Level of Care (LOC)
- Non-covered services
- Provider affiliation
- Payment not received
- Patient Liability
- Sterilization/Hysterectomy consent form
- Past Dispute Timeframe
|
12 months from the DOS or 60 days from the EOB date.
|
Disputes may be submitted via:
Phone: 1-833-644-6001 (Select the prompts for the correct department and then select the prompt for claim issues).
NaviNet portal: https://navinet.secure.force.com/ with the claims adjustment inquiry function.
Mail: The request must include a copy of the dispute resolution letter.
AmeriHealth Caritas Ohio
Attn: Provider Claim Inquiry Team
PO Box 7126
London, KY 40742
Fax: 1-833-216-2272
|
|
|
|---|
|
Access the Provider Dispute Submission Form (PDF) |
|
|---|
|
Prenatal Risk Assessment Form and Report of Pregnancy
On our provider webpage you will find a variety of resources to assist you and your practice in the care of AmeriHealth Caritas Ohio members. You will find the provider manual, guides, and policies and several ODM forms. As Ohio continues to combat the infant mortality crisis, we wanted to ensure you were aware of these forms and instructions:
|
|
We are seeking providers to serve in advisory roles
AmeriHealth Caritas Ohio (ACOH) is seeking providers to serve in advisory roles to shape the Next Generation of managed care in Ohio. Partnering physicians will provide oversight and advise on policies and programs to help patients achieve better health outcomes and reduce the administrative burden for healthcare practitioners. Compensation provided for each meeting participation. Interested in advising? Please contact Bill Walters at wwalters@AmeriHealthCaritasOH.com.
Quality Assessment and Performance Improvement Committee (QAPIC)
- Purpose: Oversight of ACOH efforts to measure, manage and improve quality of care and services delivered to members/patients.
- Meetings: Monthly, every 3rd Friday, 7 to 9 a.m. (subject to change based on provider preference). Meetings are virtual except for one in-person meeting annually.
- Materials: Delivered electronically one week prior to meeting.
- Role of external physician: participate in the Quality Improvement (QI) program through planning, design, and implementation/review of the QI program, committee/subcommittees, policy decisions, performance, etc.
- Ideal candidates: Practitioners with an interest in helping to improve the lives of Medicaid members. Specialty/background in primary care (FM or IM), maternal and infant health (OB/GYN), or behavioral health (MD, DO, PhD).
- Financial Compensation: $250 per meeting occurrence.
Provider Advisory Council
- Purpose: Input into design and improvement efforts for plan programming impacting members and providers. The council will also advise ACOH on clinical improvement efforts, determine options to reduce administrative burden, identify systematic challenges and barriers, problem-solve, share information, and collectively find ways to improve and strengthen the healthcare service delivery system.
- Meetings: Meetings will occur four times per year, generally in the last week of each quarter.
- Materials: Delivered electronically before each meeting with pre-read material usually no longer than five pages.
- Role of external physician: Provide input and feedback into design of programs and performance improvement efforts.
- Ideal candidates: Specialty/background in primary care, medical/surgical specialty, or behavioral health provider (MD, DO, PhD) with interest in learning how managed care plans develop clinical quality improvement, reduction in provider administrative burden, healthy disparity reduction efforts.
- Financial Compensation: $250 per meeting occurrence.
|
|
Mobile Wellness, meeting communities right where they are
Our Mobile Wellness and Opportunity Center can come to your community! Depending on availability and established criteria, you can work with AmeriHealth Caritas Ohio to
conduct classes, wellness events, or health education within and around the bus.
The mobile unit is equipped with kiosks where attendees can access computers and a private location where providers can perform health screenings and engage personally with members.
Working with AmeriHealth Caritas Ohio, you can increase accessibility to services that address the social determinants of life and improve conditions for members of the community. We are pleased to offer this convenience at no cost to you and your community.
For more information or to reserve time with the Mobile Wellness and Opportunity Center, click to complete the request form or email us at Comms@AmeriHealthCaritasOH.com. We welcome the chance to work with you to help people get care, stay well, and build healthy communities. |
 |
|
|
|
|
Tell us a little bit about where you’re from and where you went to school.
I grew up and went to school in Central Ohio where I still reside.
Everyone at AmeriHealth Caritas Ohio has a story about why they joined the team. What’s yours?
I found this to be an opportunity to build a network from the ground up since I worked for another MCP in Ohio for 18 ½ years building a network for them.
What drew you to this profession?
I started my insurance career in the home and auto lines of business and when the occasion presented itself in healthcare, I made the move.
What do you like to do in your free time? I like spending time with my wife and German Shepherds, golfing, and yard work. |
|
|
If you could have dinner with anyone in the world, dead or alive, who would it be? Why?
Arnold Palmer. I would discuss the game of golf and club design.
What are 2 apps on your phone you CANNOT live without?
The apps I cannot live without are YouTube and Solitaire.
Any interesting facts about yourself that you’d like to share?
I practice golf every day and play every chance I get.
Steve Babcock
Provider Network Account Executive II
sbabcock@amerihealthcaritasoh.com
Mobile: 614-400-3620 |
|
|---|
|
Beware of phishing scams — don’t take the bait!
One of the biggest information security risks for most organizations occurs when an associate opens a phishing email and clicks on the link. It only takes one associate clicking a phony link to impact an organization’s cybersecurity efforts.
|
|
|
|
|---|
|
Why it's important
Phishing scams are emails that look real but are designed to steal important information. A phishing email with malicious software can allow cybercriminals to take control of your computer and put protected health information (PHI) and personally identifiable information (PII), as well as a company’s confidential and proprietary information at risk.
It may be a phishing email if it:
- Promises something of value (e.g., “Win a free gift card”).
- Asks for money or donations.
- Comes from a sender or company you don’t recognize.
- Links to a site that is different from that of the company the sender claims to represent.
- Comes from a trusted business partner that has experienced a security incident. All emails sourcing from outside your organization should be scrutinized.
- Asks you for personal information, such as your username and password/passphrase.
- Includes misspelled words in the site’s URL or subject line.
If you suspect an email may be phishing, here are some tips:
- Do not click any links in the email.
- Do not provide your username and password; you should never share your username or password, even if you recognize the source. Phishing scams frequently mimic well-known companies, such as retailers (like Amazon) or banks.
- Do not reply or forward the email to anyone within your organization.
- Familiarize yourself with your organization’s process for reporting suspicious emails. If you suspect an email is a phishing attempt, report it immediately.
- Your organization's information security department may have additional information and guidance on how to protect yourself from phishing scams.
|
|
|---|
|
 Training opportunities Training opportunities |
|
|---|
|
Provider orientation
We encourage our new providers to attend one of our virtual orientation sessions. These offer us the opportunity to welcome you, introduce ourselves, and share our unique member benefits, value-based care program, claims and billing information and our provider portal, NaviNet. Join your personal account executives online or contact your local Account Executive to schedule an individual orientation. Click here to see the entire calendar and register.
Don't forget to complete the attestation once you attend a session. The Ohio Department of Medicaid requires us to maintain a registry for the New Provider Orientation attendance.
|
|
|
|
|
Cultural competency training
AmeriHealth Caritas Ohio is committed to promoting education on and awareness of culturally and linguistically appropriate services (CLAS) and to combatting the effects of low health literacy on the health status of our members. There are several training opportunities on our website. |
|
|---|
|
Pain Self-Management Education (PSME) is in full swing!
PSME is a four-session educational program for adults living with chronic non-cancer pain. PSME teaches pain self-management, healthy lifestyle, mindfulness, and healthy coping skills, with the goal of empowering people to live full and productive lives with pain.
This program is offered in collaboration with Meridian HealthCare at no cost to adults 18+ living with chronic pain and insured by ANY Ohio Medicaid plan.
To refer to this program, please direct patients to contact Meridian HealthCare directly at 1-330-797-0070 or email chronicpain@meridianhealthcare.net. Additional program information and referral flyers can be obtained by contacting Jhilleary@AmeriHealthCaritasOH.com.
|
|
|---|
|
Register for Provider Network Management module new features training
The Ohio Department of Medicaid, in partnership with Maximus, the Provider Network Management (PNM) module vendor, is continuing provider awareness and training efforts around the new features implemented in the Ohio Medicaid Enterprise System.
Providers will see and utilize these new features in the PNM module beginning on June 30. There is still time to register for the PNM new features training. |
|
|---|
|
2024 Comprehensive Primary Care (CPC) Webinar Series with ODM
ODM will virtually share program updates, resources, best practices, and more. They are scheduled on:
- Thursday, September 19
- Thursday, November 14
|
|
|
Ask a Sandata trainer
Do you have questions about Electronic Visit Verifications (EVV)? You can schedule a private Zoom session with a Sandata trainer to discuss your EVV questions. The sessions cover: improving claims matching, solving reoccurring exceptions, and getting started with EVV.
|
|
|---|
|
Disability Pride Month
In July, we celebrate Disability Pride Month to commemorate the passing of the Americans with Disabilities Act (ADA), a landmark civil rights law signed on July 26, 1990.
The ADA prohibits discrimination against individuals with disabilities in all areas of public life, including employment, transportation, housing and access to various government programs and services.
Disability Pride Month is also a time to uplift disability pride by promoting visibility and mainstream awareness of disabilities, which are natural parts of human diversity. Disability pride champions inclusion while challenging ableism and stigmatizing definitions of disability.
Disability, visible or invisible, can happen at any point in a person's lifetime. As individuals, we experience disability differently. Celebrating Disability Pride includes expanding our consciousness of others who may be living with disabilities and raising awareness to change how disability is perceived.
|
|
|
|
|
|  |
|
|
|
|
